by Thomas L. Kirchgessner, MAT in Biology
Neal Johnson, BS in Pharmacy, RPh

The protection is aimed at publishing this blog on the web. It is perfectly alright to download it to your computer for personal, non-commercial use. I have found that Internet Explorer 8 and Chrome 16 do a fine job, though image placeholders must be clicked in order to display images.
Table of Contents
Background for Kinetics
Things You've Heard About
Recent History of HbA1c Testing
Mathematical Relationships of HbA1c Units and Plasma Glucose Units
ADAG, A1c-Derived Estimated Glucose
Kinetics (Internal links for navigation have yet to be added for the remaining index items.)
Elementary Concepts
Defining the Time
Illustrating the Birth and Aging of RBCs with Accumulation of HbA1c
One Half Exposure to Sugar in the Month (or Day) of Birth
One Easy Mistake
Another View of HbA1c Formation, Using a Graph
Normal, Shortened, and Variable RBC Lifespan and HbA1c, a Weighted Average
Simple Case
The Last Month Reigns
Glycation of Individual Cells Compared to Grouped Cells
Short RBC Lifespan
We Don’t Know the Lifespan
HbA1c is Not an Average
A Look at Effect of Lifespan Variation with a 120 Day Mean Life
The Research Front
References
Appendix
Graph Comparing 90 and 120 Day Lifespans per Relative Numbers of Tables 4 and 5
Graph of High Sugar in the Last Month per Relative Numbers of Table 7
Graph of High Sugar in the Oldest Month per Relative Numbers of Table 6
Estimating the Effect of a Change in Therapy
Welcome to this blog. Please, feel free to leave any sort of comment at the end of the blog. If you would like to add ideas with supporting references, please do so. If you are a mathematician (I am not.), you might like to present some simple equations incorporating increase in HbA1c, lifespan, and plasma glucose concentration. You can have more complicated math in your derivation if you like, but algebraic final equations would be understood by a wider audience. If you want to incorporate loss of Hb from aging red blood cells, variable glycation index, and the "rebound effect" of hyperglycemia causing shortened RBC lifespan, I will try to direct you to some literature so that you can model realistically. Cheers, Tom K
=====================================================================
Background for Kinetics
Things You've Heard About
Recent History of HbA1c Testing
Mathematical Relationships of HbA1c Units and Plasma Glucose Units
ADAG, A1c-Derived Estimated Glucose
Kinetics (Internal links for navigation have yet to be added for the remaining index items.)
Elementary Concepts
Defining the Time
Illustrating the Birth and Aging of RBCs with Accumulation of HbA1c
One Half Exposure to Sugar in the Month (or Day) of Birth
One Easy Mistake
Another View of HbA1c Formation, Using a Graph
Normal, Shortened, and Variable RBC Lifespan and HbA1c, a Weighted Average
Simple Case
The Last Month Reigns
Glycation of Individual Cells Compared to Grouped Cells
Short RBC Lifespan
We Don’t Know the Lifespan
HbA1c is Not an Average
A Look at Effect of Lifespan Variation with a 120 Day Mean Life
The Research Front
References
Appendix
Graph Comparing 90 and 120 Day Lifespans per Relative Numbers of Tables 4 and 5
Graph of High Sugar in the Last Month per Relative Numbers of Table 7
Graph of High Sugar in the Oldest Month per Relative Numbers of Table 6
Estimating the Effect of a Change in Therapy
Welcome to this blog. Please, feel free to leave any sort of comment at the end of the blog. If you would like to add ideas with supporting references, please do so. If you are a mathematician (I am not.), you might like to present some simple equations incorporating increase in HbA1c, lifespan, and plasma glucose concentration. You can have more complicated math in your derivation if you like, but algebraic final equations would be understood by a wider audience. If you want to incorporate loss of Hb from aging red blood cells, variable glycation index, and the "rebound effect" of hyperglycemia causing shortened RBC lifespan, I will try to direct you to some literature so that you can model realistically. Cheers, Tom K
=====================================================================
A simple graphic visualization of A1c kinetics on a month by month basis points out that the hemoglobin A1c (HbA1c) test is not an average but a weighted average and that abnormalities in red blood cell (RBC) lifespan give misleading A1c values. This is presented essentially without math. But still, be prepared to concentrate. The new International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) units of millimoles of A1c to moles of adult Hb are most useful for this demonstration. The latest relationship of estimated average glucose (eAG) to HbA1c produced by the A1c-Derived Average Glucose study (ADAG) is also incorporated in the visualization. The chemistry of HbA1c formation and testing is not discussed here, but it is of first importance as there have been different assay methods which have given different HbA1c values. This tutorial is written for nurses, such as my daughter and daughter-in-law, but educators and even providers may find it helpful.
Background for Kinetics
Things You’ve Heard About or Know Better Than I. The HbA1c test is a very useful blood test for diabetics and their providers. The higher the blood glucose has been over the past two to four months, the higher the number of the HbA1c test result. It is not a replacement for home finger sticks which measure the amount of blood glucose in milligrams per deciliter (mg/dl) at points in time. It has the advantage of being sort of an “average blood glucose” over an extended time. This makes up for the lack of finger sticks through the nighttime and for days when not enough finger sticks were done. Besides that, it is a check on home finger sticks, because home glucose meters do not have the accuracy of a laboratory test. It is reported in the U.S.A. as a percent, like 6.0%. This means that 6% of the hemoglobin molecules within the red blood cells (RBCs) have sugar attached. The sugar attaches in a non-enzymatic chemical reaction. Once attached, the Hb is said to be glycated or glycosylated. (Glycation is currently the preferred term, as glycosylation implies an enzyme-aided reaction.) It is also called glycohemoglobin. It stays that way through the time blood is drawn for the HbA1c test unless the RBC dies. If there is twice as much glucose in the blood there is about twice the amount of HbA1c formed. (Neat, isn’t it.) There is an alternative to the HBA1c test called the fructosamine test. It also “averages” blood sugar over time, but for a much shorter time than HbA1c.
Now, you know there are several kinds of Hb in the blood. In healthy people, 95% or more of it is adult Hb (HbA). There is some HbA2, some fetal Hb (HbF). And there can be abnormal Hb’s like the one associated with sickle cell disease. An important glycated HbA is called HbA1, and it has three subtypes called HbA1a, HbA1b, and HbA1c. There are also other glycated Hb’s.
One HbA molecule is a monstrous protein with a molecular weight of around 68,000. (Compare to the weight of a water molecule which is 18.) It has four subunits of nearly equal size, and each subunit is a chain of many amino acids with an attached heme group which carries oxygen. Two of the chains are called alpha chains and two, beta. The chains have helical sections and are also folded upon themselves; therefore, the molecule is not spread out in a line, but is very compact.
A Bit of Recent History of the A1c Test, the Numerator and Denominator of the Glycohemoglobin Fraction. The latest international recommendations by the IFCC were developed by a working group between 1995 and 2002. These guidelines, which have not been fully implemented, include reporting as millimoles of HbA1c divided by moles of HbA. (If your chemistry is forgotten chemistry, just think of a mole as a certain amount of a chemical substance. Then a millimole would be 1/1000 of a mole. A millimole per mole is abbreviated mmol/mol.) These units can be converted to a percentage of HbA which is glycated. The recommendations produce the most accurate measure of HbA1c ever. Most importantly, the IFCC produced pure lots of HbA0 (non-glycated HbA) and HbA1c to use as reference standards. The IFCC defines HbA1c as a molecule with one or both of the beta chain N-terminal valines (an amino acid) glycated. Whether additional sites such as an alpha N-terminal valine or side chain lysines (alpha or beta) are glycated does not affect the definition. The IFCC percentage of glycation is lower than the NGSP percentage because the the latter considers HbA glycated on the alpha chain or at a beta chain lysine to be "glycated Hb." Therefore; more molecules are glycated under the NGSP method, and the percentage is accordingly higher.
In early years, glycated Hb testing was in disarray. Results varied greatly from one clinical lab to another. Some tested for HbA1c, some for HbA1, and some for all glycated Hb’s, and many different methods were used which gave discordant results, even when testing for the same substance. The National Glycohemoglobin Standardization Program (NGSP), based in the U.S.A. 1996 through the present, has corrected the unacceptable lab to lab variation. However, the NGSP “harmonizes” their excellent results to agree with the glycohemoglobin results of the Diabetes Control and Complications Trial (DCCT) study of 1983-93 . The DCCT tests were not as specific for HbA1c as the new IFCC test. The chemistry was 1983, not 2011. There were glycated Hb’s other than HbA1c in the numerator and even the denominator. Nevertheless, the NGSP produced curves relating more up-to-date methods to the exact procedures used in the DCCT lab. As an example, a true IFCC HbA1c percentage of 4.2% is harmonized to an NGSP, DCCT 6.0%. But this was really a “no-brainer.” The DCCT is a famous 10-year study which, along with a study in the United Kingdom, for the first time documented that higher glycohemoglobin was highly correlated with diabetic complications like retinopathy and neuropathy. It tied the glycohemoglobin levels to the risk of developing tissue damage and so had a great clinical value. So, harmonization produces clinically meaningful results for doctor and patient.
The NGSP and the IFCC continue to work together. This is certainly not a competition. The NGSP continues to perform a great service. I personally prefer the IFCC units, but there is a caveat. Comprehensive correlations to tissue damage were made with the DCCT chemical methods, but never say never. What if these correlations are stronger than correlations with the new, more specific, purer HbA1c test? I’ve not read anyone’s predicting this. I’ve read that HbA1c does make up 50-60% of the total glycated Hb, and people expect things to go well. (I do wonder how they define 50-60% to fit with the IFCC definitions. Presumably, they disregard the IFCC definition and refer to the fact that 50-60% of attached sugar is attached at a beta N-terminal valine and the remaining 40-50% is attached elsewhere.)
The NGSP and the IFCC continue to work together. This is certainly not a competition. The NGSP continues to perform a great service. I personally prefer the IFCC units, but there is a caveat. Comprehensive correlations to tissue damage were made with the DCCT chemical methods, but never say never. What if these correlations are stronger than correlations with the new, more specific, purer HbA1c test? I’ve not read anyone’s predicting this. I’ve read that HbA1c does make up 50-60% of the total glycated Hb, and people expect things to go well. (I do wonder how they define 50-60% to fit with the IFCC definitions. Presumably, they disregard the IFCC definition and refer to the fact that 50-60% of attached sugar is attached at a beta N-terminal valine and the remaining 40-50% is attached elsewhere.)
IFCC and NGSP results are inter-convertible through a master equation. Each country will decide whether to fully adopt the new units, to report as an NGSP, harmonized percentage, or to report using both sets of units. The U.S.A. will continue to report HbA1c as an NGSP, harmonized percentage.
The Mathematical Relationships. Figures 1 and 2 and table 1 show the inter-relationship of NGSP and IFCC HbA1c units and also of plasma glucose to HbA1c.
Figure 1. HbA1c, NGSP vs. IFCC, from the NGSP website. The IFCC is drawn as a percentage, which clearly shows the difference between the two. The conversion, using 42 mmol/mol, works like this: (42 mmol HbA1c/mol HbA) x (1 mol/1000mmol) x 100 = 4.2%, as units cancel. As a shortcut, just divide the number 42 by 10 to get the percentage.
Table 1. HbA1c and Plasma Glucose, from the NGSP Website
IFCC HbA1c (mmol/mol) | NGSP HbA1c (%) | eAG (mg/dl) | eAG (mmol/l) |
31 | 5 | 97 | 5.4 |
42 | 6 | 126 | 7.0 |
53 | 7 | 154 | 8.6 |
64 | 8 | 183 | 10.2 |
75 | 9 | 212 | 11.8 |
86 | 10 | 240 | 13.4 |
97 | 11 | 269 | 14.9 |
108 | 12 | 298 | 16.5 |
The plasma glucose-A1c relationships are those of ADAG. NGSP: eAG (mg/dl) = (HbA1c (%) x 28.7) minus 46.7, r2 = 0.84 and IFCC: eAG (mg/dl) = (HbA1c (mmol/mol) x 2.63) + 15. ADAG is discussed just a little bit after figure 2.

Figure 2. HbA1c in percentage vs. plasma glucose in mg/dl, per ADAG. The IFCC is presented as a percentage to clearly show the NGSP-IFCC difference.
Please, notice that double the glucose level produces a little less than twice the HbA1c in NGSP percentage, but a little more than twice the HbA1c in mmol/mol. Take a look at table 1.
A glucose of 97 mg/dl produces 5.0% HbA1c, but if we double this to 194 mg/dl, the HbA1c will be between 8.0% and 9.0%, not 10.0%. In the same vein (yes, I admit it), the 31 mmol/mol becomes 68 mmol/mol, not 62. All of this is because the lines don’t cross the axes at
x = 0, y = 0.
ADAG, the Relationship between HbA1c and Estimated Average Blood Glucose. The latest determination of this relationship was made by the A1c-Derived Average Glucose Study (ADAG), 2006-2008.(1) It was sponsored by the American Diabetes Association (ADA), the European Association for the Study of Diabetes, and the International Diabetes Federation. It was a large 16-week study of over 500 stable subjects which included type 1 and type 2 diabetics and non-diabetics. Seven to eight daily fingersticks done by the subjects, periods of continuous interstitial monitoring, and A1c tests were all evaluated. Many measures of glycemic control and their interrelationships were analysed. The resulting estimated average blood glucose is abbreviated eAG. The study is considered superior to a similar part of the DCCT study. Their equations are shown in table 1. The ADA recommends reporting of the eAG along with the NGSP percentage. I emphasize that it is called “estimated” for good reasons. To me, the 95% percent prediction intervals are large. At 97 mg/dl plasma glucose the interval is 76-120, and for 298 mg/dl it is 240-347 mg/dl. There are many conditions which throw a monkey wrench into this estimation. Best to consult your physician or nurse practitioner. Also, Tri Core lab results do not precisely follow this table as of 3-1-11, per the lab report on my own A1c test.
Mini-tutorial on Confidence Limits. At a five percent NGSP value for HbA1c, RBCs were exposed to an average 97 mg/dl of plasma glucose (table1). But some people had greater than 97 mg/dl and some less than 97 mg/dl at 5% HbA1c The prediction interval is calculated mathematically, and it shows (almost) that the researcher is 95% sure that the long-term average plasma glucose of an untested individual will lie between 76 mg/dl and 120 mg/dl if his HbA1c is 5%. Let's illustrate the prediction interval with an everyday example. Suppose that you know that men's heights average 5'10". How sure would you be that the next guy you see is between 5'9" and 5'11"? Not very sure! You might have 10% confidence in that interval. However, you might be 95% sure that he will be between 5'5" and 6'3". You might even be 99.999% certain that he will be between 4'6" and 7'2". And then Yao Ming (7'6" basketball player from China) comes along. That's life! The difference is that you are guessing and the researcher is calculating.
Kinetics
Elementary Concepts
Defining the Time. The time of sampling defines all of the time units used in this tutorial. Sampling is always done at zero time of day #1. Then, we count backwards in time to get one day old, 120 days old, day #120 , and so forth. All months are 30-day months.
Let’s say we sample at 11:59.99999 p.m. on April 30. The four months then are Jan.1-30, Feb. 1-30, Mar. 1-30, and Apr. 1-30. Day #1 is Apr. 30 and day #120 is Jan. 1. (Feb. 30th. You like that?) I will refer to them as the month before the sampling, the second month before, and so on. Time zero is at 11:59.99999 p.m. of Apr. 30 and time 120 days, i.e., 120x24 hours is at the beginning of Jan.1.
Day # Day #120 Day #2 Day #1
1------------1---------------- - - -------------------------1------------1------------1-------------1
Time 120 d 119 d 2 d 1 d 0 d
Illustrating the Birth and Aging of RBCs with Accumulation of HbA1c. There are about 2.4 million RBCs born per second. In these illustrations. One RBC will stand for all of the RBCs born on a particular day. To make it practical, there will be only four days in a month. We are going to follow some new RBCs and ignore all of the RBCs already present in the blood stream. The sugar concentration will be designated by a color so that 2sug or 1sug would be amounts of HbA1c formed under the orange sugar concentration and 1sug would be an amount formed under the blue concentration. (Of course, these concentrations are some amount of glucose in mg/dl.) To make my model work, any change in sugar concentration must occur exactly as a new month is starting. (A day by day model could be used for changes in the middle of the month.) Remember, I’m counting backward, so day #8 is the oldest day.
Do a quick study of all the tables as though they were mini-spreadsheets. Compare them to each other. Let’s get hoppin’ with table 2.
Table 2a. Birth and Aging of RBCs, 2nd Month Ago, cumulative amount of HbA1c
Sugar conc | RBCs | Birthday | Day #8 4-23 | Day #7 4-24 | Day #6 4-25 | Day #5 4-26 |
orange | Neal | 4-23 | 1/2sug | 1 1/2sug | 2 1/2sug | 3 1/2sug |
orange | Aaron | 4-24 | 1/2sug | 1 1/2sug | 2 1/2sug | |
orange | Veena | 4-25 | 1/2sug | 1 1/2sug | ||
orange | Shayla | 4-26 | 1/2sug | |||
Total 8sug |
Why the One Half Exposure to Sugar in the Month (or Day) of Birth? Understanding this is crucial to accepting my figures. Let’s think “by the month” here. An RBC born at the very beginning of the month will have 30 days of exposure to the blood sugar level of that month. One born at the exact middle of the month will have 15 days, and one born at the last second will have zero exposure. So the average exposure is one half month. But then the new month instantly begins, and all the cells we are speaking of will then be exposed to the new month’s concentration for the following 30 days, so that the average exposure is a full month. The “by the day” view is analogous.
Table 2b. 1st Month Ago, cumulative amount of HbA1c
Sugar conc | RBCs | Birthday | Day #4 4-27 | Day #3 4-28 | Day #2 4-29 | Day #1 4-30 |
blue | Neal | 4-23 | 3 1/2sug1sug | 3 1/2sug2sug | 3 1/2sug3sug | 3 1/2sug4sug |
blue | Aaron | 4-24 | 2 1/2sug1sug | 2 1/2sug2sug | 2 1/2sug3sug | 2 1/2sug4sug |
blue | Veena | 4-25 | 1 1/2sug1sug | 1 1/2sug2sug | 1 1/2sug3sug | 1 1/2sug4sug |
blue | Shayla | 4-26 | 1/2sug1sug | 1/2sug2sug | 1/2sug3sug | 1/2sug4sug |
blue | Jessica | 4-27 | 1/2sug | 1 1/2sug | 2 1/2sug | 3 1/2sug |
blue | Rod | 4-28 | 1/2sug | 1 1/2sug | 2 1/2sug | |
blue | Lauren | 4-29 | 1/2sug | 1 1/2sug | ||
blue | Allyson | 4-30 | 1/2sug | |||
Total | 8sug24sug |
Table 3. Table 2 in a Different Format, not cumulative
Birth month of RBCs | A1c made 2nd m ago | A1c made 1st m ago | Total HbA1c |
2nd month ago | 8sug | 16sug | 8sug16sug |
1st month ago | 8sug | 8sug | |
Total HbA1c | 8sug | 24sug | 8sug24sug |
One Easy Mistake. To visualize that there is a line of cells marching single-file from an orange environment into a blue environment is in error. See pictorial 1. After all, all living cells are exposed to the same blood sugar at any one time. To make my model work, any change in sugar concentration must occur exactly as a new month is starting. Of course, this is unrealistic, but this is only a model--have mercy. If it were necessary to consider concentration changes in the middle of the month, then a day by day view would be appropriate.

Pictorial 1. Erroneous way to visualize glycation of cells born days #6 to #1, after 6 days. Under the simplified 4 d per month scheme.
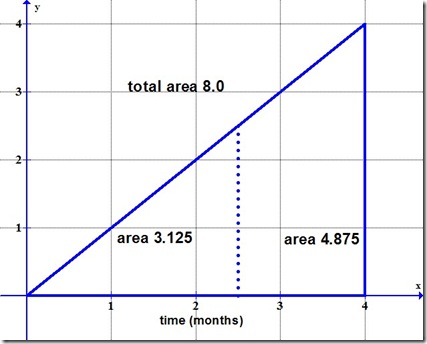
Another View of HbA1c Formation, Using a Graph. Figure 3 shows HbA1c formed over time in new RBCs at constant sugar level. It shows table 3 data graphically for the case where there has not been a change in sugar level, ie, orange equals blue. Time progresses to the right and is in continuous units of days, so that 12 hours would be at 0.5 d, 24 hours at 1 d, and so forth. The red line is the increasing rate of glycation as more cells are born, and the area is the amount of HbA1c in arbitrary units.

The areas of the triangles are the integrated areas under the straight red line, y = x, from 0 to 4 and from 0 to 8 d. The integral is Y = x2/2. (x2 is x squared.) If table 3 had only one sugar level instead of two, it would match figure 3, because both would show that 24/32 of the total A1c is formed during the more recent month.
Normal, Shortened, and Variable RBC Lifespan and HbA1c, a Weighted Average
Simple Case. Again, we are going to follow some new RBCs and initially ignore all of the RBCs already present in the blood stream. All of these old RBCs will die by the time of the blood draw. We’ll look at the HbA1c formed in new RBCs month by month during the four months preceding the HbA1c assay. Let’s use simplifying assumptions. (1) Assume that every single RBC has a 120 day, 120x24 h lifespan. (2) Let the average daily blood sugar be constant. (3) Have the rate of HbA1c formation over time be constant at the level of an individual RBC. Rate of formation will evenly increase, however, when we are looking at all the new cells collectively. This is because RBCs are continuously born so that the group continuously becomes larger so that there is more and more HbA exposed to sugar -- yep, continuously. (4) Have all other relevant features of the blood, such as Hb level and RBC count, be constant, blah, blah, blah. Assume the patient is really healthy or has early diabetes in an otherwise healthy body. In this simple case the plasma glucose is 126 mg /dl, HbA is 15 g/dl, and NGSP HbA1c is “6.0%." Please, see figure 2 and table 1 for the plasma glucose vs. HbA1c fit. The IFCC mmol/mol is 42 which is a true percentage of 4.2
NGSP = (42 x 0.0915) + 2.15 = 3.843 + 2.15 = 5.993 = 6.0%
Table 4 shows the amount of HbA1c in RBCs “born” the month preceding the sampling, in RBCs born the second month preceding the sampling, and so on for the third and fourth months. Note that I did not say RBCs one month old, two months old and so on because for each month only the cells of one day or hour or minute would be exactly so many months old. The total HbA1c within cells is compared by the birth month, and this same total is also allocated to the month in which it was formed. You don’t see the 42 mmol/mol until the grand total as it takes the whole four months to form this amount
Let me further clarify the figures. The 5.25 mmol/mol figure at the 4th month-3rd month intersection means that 5.25 mmol/mol of HbA1c was formed from 60 to 90 d ago in cells born the fourth month ago . The denominator is the number of moles of HbA in the whole circulatory system. If you want a denominator of moles of HbA inside the cells born the fourth month ago, then multiply the 5.25 by 4.0 giving you an answer of 21.0 mmol/mol. (Using the “old slide the decimal point one place to the left trick,” you see that 2.1% (true percentage) of the HbA in any 4th month cell was glycated during the month.)
Table 4. HbA1c Formation and Assay, Simple Assumptions, mmol/mol HbA1c, non-cumulative
Birth month of RBCs | A1c made 4th m ago | A1c made 3rd m ago | A1c made 2nd m ago | A1c made 1st m ago | Total HbA1c |
4th month ago | 2.625(b) (a) 1/2 | 5.25 1 | 5.25 1 | 5.25 1 | 18.375 3 1/2 |
3rd month ago | 2.625 1/2 | 5.25 1 | 5.25 1 | 13.125 2 1/2 | |
2nd month ago | 2.625 1/2 | 5.25 1 | 7.875 1 1/2 | ||
1st month ago | 2.625 1/2 | 2.625 1/2 | |||
Total HbA1c | 2.625 1/2 | 7.875 1 1/2 | 13.125 2 1/2 | 18.375 3 1/2 | 42.00 8 |
Table 4 shows that the RBCs of birth month four contribute much more to the HbA1c value (18.375 mmol/mol) than those of any other birth month. In a seeming contradiction, the HbA1c formed in the first month ago (18.375 mmol/mol) is much greater than that formed in the fourth month ago. We will discuss these two issues later.
The only cells shown in table 4 are the cells which will be in the sample. The missing cells are those born the fifth, sixth, seventh, and eighth months ago. You could fit parts of months five through seven into the empty areas in table four, although logically each should have a row of its own. You can notice in the “A1c made 1st month ago” column that 3 1/2 relative units of HbA1c were made. Additionally, 1/2 unit goes into dying cells born the 5th month ago. Therefore, 4 units would be made every month, since constancy is one of our simple assumptions. Figure 6 illustrates this constancy. One more comment on the table. It can represent steady state when “months ago” is redefined at the end of each 30 days.
I have two sweet graphs, figures 4 and 5, that redundantly illustrate the numbers of table 4. You may find them more meaningful than the table. The line, y = x, shows the rate of formation of HbA1c, not the amount. It rises because of unending births of new RBCs. The amount of HbA1c is the area under y = x. It is drawn with the relative units of table 4. The triangle has a total area of 4 x 4 / 2, i.e., 8 square units which is the grand total of table 4.

Figure 4. This graph shows the HbA1c content of surviving RBCs by cell age. It duplicates information of table 4. The A1c amount is area, as in figure 3. The integral, Y = x2/2 is the area from x = 0 to x = whatever. It agrees with the area under y = x from x = 0 to x = whatever.. Notice that there are 6 full colored rectangles and 4 half rectangles under y = x. This total of 8 units is the Y value of Y = x2/2 at 4 months, and 8 is also the area from x = 0 to x = 4. The units on the y axis do not fit “Y = x2/2,” as Y is not a rate (per month), but an amount. The y axis would be labeled just “HbA1c arbitrary units” in order to apply to Y = x2/2.

Figure 5. This graph shows when the surviving HbA1c was made. A1c amount is area, as in figure 3. Note the great amount made in the last month which is the area under y = x from x = 3 to x = 4. This amount is 3 1/2 units, ie, the number of rectangles between x = 3 and x = 4. How about the rate of formation at 3 months? This is the point, x = 3 and y = 3, and it means that at precisely 3.0000 months, the rate of formation is 3.0000 units/month.

Figure 6. This figure illustrates that 4 units of HbA1c are made every month. The graph is showing continuous time. What would we see if we looked in a very narrow window at 3.00 months? Bottom to top, we would see 4th month ago, 3rd m, 2nd m, and 5th month ago. And how about at 3.50 months: 4th m, 3rd m, 2nd m, 1/2 of last m, and 1/2 of 5th m. I hope you now have a complete understanding of the construction of these graphs.
The Last Month Reigns. It is no secret that the HbA1c assay is a weighted average with more recent blood glucose levels contributing much more than earlier levels. "Thus, a large change in mean blood glucose is accompanied by a large change in GHb within a matter of 1–2 weeks, not 3–4 months . In effect, GHb is a “weighted” measure of mean blood glucose during the preceding 120 days; more recent past events contribute relatively more to the final result than earlier events. The mean level of blood glucose in the 30 days immediately preceding the blood sampling (days 0–30) contributes ∼50% to the final result, whereas days 90–120 contribute only ∼10%." This statement is from David E. Goldstein, et al, in 2004. (9)
The relative effect of the four months of HbA1c formation upon the HbA1c assay abides by the ratio of 7:5:3:1 for months of A1c production 1,2,3,and 4. This ratio is the ratio of the areas in figure 5. Let me emphasize that the dominance of the last month prevails whether HbA1c formation is constant for the four months or whether it varies. If therapy has greatly improved glycemic control in the last month, i.e., the 1st month ago, this last month will show its dominance by its lack of A1c production. Let’s illustrate. Say that high sugar in months 2 to 4 was at a level which would after four months produce a harmonized NGSP of 10%. Also, we’ll say that the sugar level improved so that the last month’s level would have produced a harmonized NGSP of 7% if it had been existent for four months. The assay will show a harmonized NGSP of 8.7%. This would be a golden, no platinum, bit of clinical information. The calculation is shown below:
Month ago 1 2 3 4 Total
Projected A1c 7% 10% 10% 10%
Weight x7 x5 x3 x1 16
Product 49 50 30 10 139
A1c = 139 / 16 = 8.7%, harmonized NGSP. The unweighted average is 37 / 4 = 9.25%. The last two months at 7% gives a weighted 7.8%, unweighted 8.5%.
The same weighting should work after converting NGSP harmonized percentage to mmol/mol. Ten percent NGSP = 85.8 mmol/mol, and 7% NGSP = 53.0 mmol/mol. Let’s test it:
Month ago 1 2 3 4 Total
Projected A1c 53.0 85.8 85.8 85.8
Weight x7 x5 x3 x1 16
Product 371 429 257.4 85.8 1143.2
1143.2 / 16 = 71.45 mmol/mol. NGSP = (.0915 x IFCC) + 2.15 = (.0915 x 71.45) + 2.15 = 8.69% NGSP. We have the identical answer
.
Glycation of Individual Cells Compared to Grouped Cells. Figure 7 shows the percentage of glycation of individual cells over time as ((HbA1c in the cell) / (HbA in the cell)) x 100. A cell is born at the lower left of a line and moves upward and to the right, gaining HbA1c unceasingly. Each cell has just the smallest amount more of HbA1c than the cell to its left The cell just born has 0% A1c while the oldest cell has the maximum amount at its particular sugar level. The blue line has greater slope and a higher HbA1c percentage than the red line. Any group of evenly spaced numbers; like 0,1,2,3,4,5; has an average of (the top number plus the bottom number) / 2. This is easier than summing all of the numbers in the group. Therefore, the average glycation of cells in the blue line is (16% + 0%) / 2 = 8%. Thus, 8% is the average glycation and also the glycation of the cell in the middle which is 60 days old. By constant sugar concentration, I merely mean that the average level for one day is about the same as that for all other days. I know that the sugar level goes up after meals and then down, and down with exercise and insulin. These fluctuations do not keep the level from being constant in a broad sense.

Figure 7. A graph showing how much of the HbA in individual cells is glycated as the cells age.
The idea for this graph comes from Dr. Mahdi Kahrom, an Iranian cardiothoracic surgeon.(2)
Figure 8 marks the average glycation for cells aged 0 to 1 month, 1 to 2 months, and so on. Again, the midpoint of a group of cells gives us the average. Please, see that the overall midpoint gives us the same HbA1c percentage that the blood test will give. Note that the youngest month glycates only 2%, half of the 4% increase of the other months. This is another reminder that the birth month glycates only half the amount of other months. The relative amount of HbA1c carried by cells born the 4th month ago through the most recent month is obviously 14:10:6:2 or 7:5:3:1 (figure 8), as previously stated. How would we get the figures for the amounts formed in the most recent month through the 4th month ago? We’ll have to play with figure 8.

Figure 8. A graph showing the average glycation of cells by age and the HbA1c percentage of the assay.(2)
Imagine that we take the cells of figure 8 back four months so that the 120-day-old cells are just beginning to show in the graph. In the first month, onward from that point, they will have an average 2% glycation. So, there is 2% glycation in the 4th month ago. Then, in the 3rd month ago these cells will advance from 2 to 6% glycation for a gain of 4%, and the cells behind them will glycate the 2%. This totals 6% formed in the 3rd month ago. Likewise, the formation in the 2nd month ago and the most recent month will be 4% + 4% + 2% = 10% and 4% +4% + 4% +2% = 14%. So the ratio is also 7:5:3:1 for A1c formed in months from the most recent to the 4th month ago. Same as in the tables, of course.
The last graph in this series, figure 9, shows the individual and grouped glycation in the same figure. It is necessary that the mean individual percent in figure 9 match the total area of the grouped cell graph, since the latter is drawn in percentage. Es correcto. There is also a match of individual months. For instance, we can add 14 + 10 + 6 + 2 = 32 and then divide 14 by 32 to see that 43.75% of the glycation occurs from 3 to 4 months in time. The area of the triangle from 3 to 4 months forms a trapezoid of area (4 + 3) / 2 x (an altitude of 1) = 3.5. Then, 3.5 / 8 = 43.75%. Identical.

Figure 9. Illustrating the comparability of two graphic methods. At the end of four months, each method shows that 8% of the total HbA in the body is glycated. This total HbA is the sum of the non-glycated, the HbA0, and the glycated, the HbA1c. However; before four months the methods give different numbers. Both numbers are correct, but they have different meaning. Let's look at 2 m. With the individual cell presentation, we would average all the cells from zero to two months of age and obtain 4% as the mean percentage glycation of the HbA within these same cells. With the grouped cell presentation, the area from x = 0 to x = 2 is 2 x 2 / 2 = 2%. This number is only half as large. Remember that in the tables and in the graphs derived from them, like figures 4 and 5, the denominator is not the HbA within the cells of interest but instead is the HbA within the entire circulatory system. This denominator is twice the size and so the quotient is only half as large. Whew! That was tough. Please, look right below.
Period mean % glycation within Conversion % of whole-body
(m) individual cells factor HbA glycated
0-1 2 1/4 1/2
0-2 4 2/4 2
0-3 6 3/4 4 1/2
0-4 8 4/4 8
Short RBC Lifespan. Let us consider a patient with shortened RBC lifespan. Make it really good: no birth month four. Make it even better: no one has yet detected this abnormality.
His RBCs have a uniform 90-day lifespan. He is missing those RBCs which contribute so much to the test result. We will keep most assumptions of the simple case except this patient is not healthy as he has some sort of hemopathy. Just cross out the top row of table 4 and redo the additions, as in table 5. Each value must be multiplied by 4/3 because the lifespan has decreased by 1/4. (Please, see the appendix for a complete explanation.) He will have a test result of 31.5 mmol/mol of HbA1c. Comparison of tables 4 and 5 shows a 25/100 reduction of the IFCC from 42mmol/mol to 31.5.
As verification of the 25/100 decrease, just consider that with a 90 d lifespan and a mean cell age of 45 d, only 3/4 as much A1c in percent will form as in a 120 d lifespan and a mean cell age of 60 d. Please, see figure 10 for an illustration. The y axis is the percentage of the HbA in a single cell which is glycated. Note that the 6% glycation is 3/4 of the 8% glycation.

Figure 10. Three month vs. four month lifespan. Current belief is that individual RBCs accumulate HbA1c uniformly as they age. The mean percent is half the percent in the oldest cell.(2) The mean percent of HbA1c in the zero-to-90 day old cells is only 3/4 that of the zero-to-120 day old cells.
Table 5. HbA1c Formation and Assay, Missing 4th Month, mmol/mol HbA1c,
non-cumulative.
Birth month | A1c made 4th m ago | A1c made 3rd m ago | A1c made 2nd m ago | A1c made 1st m ago | Total HbA1c |
4th month ago | xxxxxxxxx | xxxxxxxxx | xxxxxxxxx | xxxxxxxxx | xxxxxxxxx |
3rd month ago | xxxxxxxxx | 2.625 x 4/3 1/2 x 4/3 | 5.25 x 4/3 1 x 4/3 | 5.25 x 4/3 1 x 4/3 | 17.5 3 1/3 |
2nd month ago | xxxxxxxxx | 2.625 x 4/3 1/2 x 4/3 | 5.25 x 4/3 1 x 4/3 | 10.5 2 | |
1st month ago | xxxxxxxxx | 2.625 x 4/3 1/2 x 4/3 | 3.5 2/3 | ||
Total HbA1c | xxxxxxxxx | 3.5 2/3 | 10.5 2 | 17.5 3 1/3 | 31.5 6 |
Using the 31.5 mmol/mol we can go to table 1 or figure 1 to arrive at an NGSP HbA1c of 5.0% (reduced from 6%). Or, NGSP could be calculated “on its own” as a 1/4 reduction from 6.0% to 4.5%. I don’t know which way to go, as calibration curves have not been done with short-lived RBCs. Worse, a patient with a NGSP HbA1c of 10.0% would have a test result of 8.0% using the calibration curve or 7.5% “on its own." The corresponding millimole figure is also way off. Such a way-off result would not be accepted as the doctor or practitioner would disqualify the patient from A1c testing because of other tests and observations. But perhaps results from a 3 1/2 month lifespan would be accepted. (I have manipulated the equations in figure1 and table 1 to arrive at a relationship for the 90 d lifespan: NGSP90% = (0.0915 x IFCC90 mmol/mol) + 1.61. This gives NGSP percentages of 4.5 and 7.5% for the two uncertain values.)
We Don’t Know the Lifespan. Really, I have not found a definitive study on human RBC life, its mean and variation, using either radioactive or biotin tagging. One often reads “90 to 120 days” for the average, i.e., the mean. I don’t think they know exactly. My guess is that it is between 90 and 120 days. I quote from Abstracts of the Annual Meeting of the Population Approach Group in Europe in 2010. (3)
The lifespan of red blood cells (RBCs) is unknown. The primary methods for determining RBC lifespan involve labelling with a radioactive marker. Two labelling techniques have been developed: cohort labelling, where cells of a certain age are labelled, and random labelling, where all cells present at a moment in time are labelled. ….. All current labelling methods contain significant flaws including loss of the label from viable RBCs or reincorporation of the label into new RBCs after the death of the originally labelled cells.The above quote should have mentioned the biotin labelling method, which although losing some label gives an accurate count in the flow cytometry measurements used in the technique. Cohen, et al, using biotin-labeled RBCs found a combined range of mean RBC age
(not lifespan) of 38.4 to 59.5 days in a study of six diabetics and six hematological normal non-diabetics.(4) Overall mean was 49.3 days with a standard deviation of 6.3 days. (There was no significant difference of mean RBC age between the diabetics and the normal subjects.) “…patients with otherwise identical diabetic control could have very different HbA1c levels of 0.075 and 0.099 if they happened to have mean RBC ages of 38.4 and 59.5 days, respectively. These differences are of a magnitude that would affect management decisions.” Dr. Cohen is a medical doctor.
In addition to Dr. Cohen’s short estimate, Kalicki, et al, modeled lifespans of only 75.4, 87.5, and 91.8 days.(5) But, there are references to longer lifespans using the alveolar carbon monoxide method. Furne,et al, found that the RBC lifespan of 40 healthy volunteers averaged 122 +/- 23 days.(6) All of these disparate results were from normal people. What a conundrum! We must wait for the investigators to determine the pitfalls and limitations of the various methods and to come to some kind of consensus.
You can say, “What does it matter. As long as the inter-person variation is constant and the intra-person variation is low we have reliable correlations of HbA1c to average plasma glucose and other meaningful measures, even if the population mean life is 3.5 months.” Then the cynic counters that we don’t know this variation. Yet, there is truth in what you say. It is helpful just to be aware that with many Hb variants, spleen problems, some anemias, liver disease, kidney disease, blood loss and transfusion, late pregnancy, and other documented conditions a usual interpretation of HbA1c is contraindicated.
HbA1c is Not an Average. Whadayamean, not an average? Didn’t we figure eAG from A1c and vice-versa? Well, yes we did. But in the ADAG studies patients with stable A1c were selected. No one had to average greatly different monthly blood sugars--just normal daily fluctuation. We have seen above and will see again below that recent blood sugar levels have a much greater effect upon A1c than levels three months earlier. Tables 3-5 have already shown that much more surviving HbA1c is formed in the most recent month than in any older month. The section, “The Last Month Reigns,” has quantified the relative effects of the four months
--subject to the truth of the simplifying assumptions.
Is there a sense in which A1c is determined by the average glucose? Yes, there is. I can think of two cases. (1) Over a short time, like a day, if patient A has a glucose running
from 80mg/dl to 180 mg/dl, averaging 130mg/dl while patient B runs from 100 to 160 mg/dl, averaging 130mg/dl, the two will accumulate about the same amount of A1c during that day. This is because the glucose vs. A1c curve is linear. If that happens every day for months, then the two will have about the same A1c test result if there are no unusual conditions. This would be called stable plasma glucose. Stable glucose levels predict A1c, as in eAG. However, we cannot average entire months as tables 6 and 7 illustrate, unless the glucose level is more or less constant. This is because recent levels of glucose have more effect than earlier levels. (2) The second case is at the level of an individual RBC. An RBC, being quite mindless, just goes along accumulating A1c for its whole life. It knows nothing about HbA1c tests.
 If exposed to a constant glucose level it will accumulate twice the HbA1c by two months of age as it had at one month of age. It is a linear relationship. And as sugar levels change, that one RBC will gain HbA1c more quickly at a high than at a low level. If exposed to 126 mg/dl for an hour and then 166 mg/dl for an hour, it will gain the same amount of HbA1c as it would at 146 mg/dl for two hours. A perfect average. Again, it responds in a linear fashion. Assuming all his friends are as well behaved, what is the problem for the A1c test? The problem is that RBCs die, some before the next A1c test, and that others are born just before the test and have little A1c.
If exposed to a constant glucose level it will accumulate twice the HbA1c by two months of age as it had at one month of age. It is a linear relationship. And as sugar levels change, that one RBC will gain HbA1c more quickly at a high than at a low level. If exposed to 126 mg/dl for an hour and then 166 mg/dl for an hour, it will gain the same amount of HbA1c as it would at 146 mg/dl for two hours. A perfect average. Again, it responds in a linear fashion. Assuming all his friends are as well behaved, what is the problem for the A1c test? The problem is that RBCs die, some before the next A1c test, and that others are born just before the test and have little A1c. So we are testing RBCs of all ages. Only a few in the syringe were alive months ago to reflect the sugar level of those “ancient times,” but all are alive on the day of the blood draw and will reflect today’s level. On a day by day basis--and this is true--the day before the blood draw is represented 119 + 0.5 times (i.e., 239 times) more than the oldest day (i.e., day #120).
0.5
Now we’ll get down to brass tacks. Let me return to the simple case, except we will vary the plasma glucose in tables 6 and 7. Starting with table 4 let us double the plasma glucose to 252 mg/dl during the whole of the fourth month ago. Then for the third through first months, leave it at the 126 mg/dl of table 4. The total HbA1c will be changed to 45.005 mmol/mol, an increase of 3.005 or 7/100 (table 6). Converting to NGSP % using the NGSP-IFCC curve (figure 1) gives a 5/100 increase of NGSP HbA1c to 6.3%, an increase of 0.3. Not terribly significant. Now let us increase just the first month before the assay to 252 mg/dl, keeping the second, third, and fourth months before at the values in table 4. Please, see table 7. The total HbA1c goes to 63.035 mmol/mol, an increase of 21 (50/100), and conversion using the NGSP-IFCC curve shows an NGSP increase to 7.9% from 6.0% (an increase of 32/100). Very significant. In both tables the average plasma glucose is 157.5 mg/dl, but the results are very different. Please, do not try to find these HbA1c values, with 157.5 mg/dl, from the ADAG table, as ADAG studied stable glucose. That is the whole point. If a 50% increase seems very disparate from a 32% increase, please, do look at the ADAG table and note that when IFCC increases to 64 from 42mmol/mol (52%), NGSP goes from 6.0% to 8.0% (only a 33% increase).
We have seen that contributions of months 4 through 1 have the ratio of 1:3:5:7, respectively. These are the weights in a weighted average. It seems that, indeed, only the two most recent months of four have much affect on the HbA1c. If a patient will keep an interpretable daily log, per provider instructions, study of this log by the diabetes nurse will be more useful than the HbA1c for the third and fourth months back. This would take a lot of coordination. As a patient myself, I do not know that I would have the self discipline to make a really useful log. It is hard to be a guinea pig.
Table 6. High Sugar During the 4th Month, mmol/mol A1c, non-cumulative
Birth month | A1c made 4th month ago | A1c made 3rd month ago | A1c made 2nd month ago | A1c made 1st month ago | Total HbA1c |
4th month ago | 5.63 1.07 | 5.25 1 | 5.25 1 | 5.25 1 | 21.38 4.07 |
3rd month ago | 2.625 1/2 | 5.25 1 | 5.25 1 | 13.125 2 1/2 | |
2nd month ago | 2.625 1/2 | 5.25 1 | 7.875 1 1/2 | ||
1st month ago | 2.625 1/2 | 2.625 1/2 | |||
Total HbA1c | 5.63 1.07 | 7.875 1 1/2 | 13.125 2 1/2 | 18.375 3 1/2 | 45.0 8.57 |
Sugar conc | 252 mg/dl | 126 mg/dl | 126mg/dl | 126 mg/dl | aver 157.5 mg/dl |
The weighted average of table 6 is calculated below:
Month ago 1 2 3 4 Total
Sugar conc 126 126 126 252
Weight x7 x5 x3 x1 16
Product 882 630 378 252 2142
Weighted average sugar concentration = 2142 / 16 = 134 mg/dl.
mmol/mol = (eAG - 15) / 2.63 = (134 - 15) / 2.63 = 45.2 mmol/mol
And now for the NGSP weighted average:
NGSP: (HbA1c (%) = (eAG+46.7) / 28.7) = (134 + 46.7) / 28.7 = 6.3%, and
NGSP = (.0915 x IFCC) + 2.15 = (.0915 x 45.2) + 2.15 = 6.3%.
Perfect.
Table 7. High Sugar During the 1st Month, mmol/mol A1c, non-cumulative
Birth month | A1c made 4th month ago | A1c made 3rd month ago | A1c made 2nd month ago | A1c made 1st month ago | Total HbA1c |
4th month ago | 2.625 1/2 | 5.25 1 | 5.25 1 | 11.26 2.14 | 24.385 4.64 |
3rd month ago | 2.625 1/2 | 5.25 1 | 11.26 2.14 | 19.135 3.64 | |
2nd month ago | 2.625 1/2 | 11.26 2.14 | 13.885 2.64 | ||
1st month ago | 5.63 1.07 | 5.63 1.07 | |||
Total HbA1c | 2.625 1/2 | 7.875 1 1/2 | 13.125 2 1/2 | 39.41 7.49 | 63.0 12.0 |
| Sugar conc | 126 mg/dl | 126 mg/dl | 126 mg/dl | 252 mg/dl | aver 157.5 mg/dl |
The weighted average for table 7 is calculated below:
Month ago 1 2 3 4 Total
Sugar conc 252 126 126 126
Weight x7 x5 x3 x1 16
Product 1764 630 378 126 2898
Weighted average sugar concentration = 2898 / 16 = 181 mg/dl.
mmol/mol = (eAG - 15) / 2.63 = (181 - 15) / 2.63 = 63.1 mmol/mol
A Look at Effect of Lifespan Variation with a 120 Day Mean Life. There are three kinds of variation that concern a biologist. The broadest is inter-person variation. How do John’s readings compare to Maria’s and Eduardo’s and Bet’s and thousands of others in the general population? This is probably the most important variation in a study of HbA1c. If John’s test result is different from the usual results of most other persons, can we assign a reason, can we interpret his test result? This is the reason labs have a normal range for test results. It takes the knowledge of a medical doctor or practitioner to make interpretations, based upon understanding the patient’s whole health profile. A second kind of variation is intra-person variation. Does Bet give the same result Thursday that she gave on Tuesday or a month before. This is also an important variation. Inter- and intra-person go hand-in-glove. There is a third, more microscopic variation. An example is the variation among the red blood cells within one person. What are their different sizes and ages and shapes? Of specific concern in this tutorial is the question, “Do red blood cells have a range about their mean lifespan which could greatly alter HbA1c results?”
Researchers will get closer to the truth on the question of mean RBC lifespan and its variability and also on the “microscopic” variation between individual RBCs simultaneously circulating within one person. That is Science. It never has the whole truth, but it gets more and more over time. There has been some question about the degree of random RBC death that accompanies the undoubted age-related destruction of RBCs. Much more sophisticated modeling than I am presenting shows that incorporation of random destruction into an age-related model makes for a better fit to experimental data.(5) “Conclusions: Our preliminary work confirms the presence of both mechanisms (lifespan and RDR) responsible for the natural elimination of RBC. The implementation of the transit compartment model using the maximum allowed number of compartments with RDR linearly increasing over time showed to be superior and needs to be considered in future.” (RDR is random destruction rate.) The same people modeled experimental data of three researchers and derived estimated mean lifespans of 75.4, 87.5, and 91.8 days.
How often do macrophages chew up a young good-looking RBC instead of waiting for it to apply for social security? I can’t answer this, of course, but I can model a hypothetical variability by using normal distributions with greater or lesser variance, determining if the survival predicted would significantly affect HbA1c results. I’ll say ahead of time that with a 120-day mean life even with a large standard deviation of 10 days, HbA1c results would hardly change. Please, see figure 11 and table 8. All values are those we started with in table 4, except for the variation in lifespan. (The standard deviation measures how spread out the numbers are. The numbers 9, 10, and 11 have a mean of 10, and so do the numbers 5, 10, and 15. But, the standard deviation of 5,10, and 15 is greater than the standard deviation of 9, 10, and 11 because the numbers are more spread out.)
My analysis was fairly straightforward. Figure 11 predicts the death and survival of any group of cells born within a very narrow time range. (Within one minute would be a practical way to envision this.) The survival curve is cumulative, the normal curve is not. If the cells were born 151 days ago (i.e., h/24 = 151) , the graph shows that none are alive at the present time which is the time of sampling. Likewise, all of the cells born 89 days ago (i.e. h/24 = 89) are still alive. One-half the cells born 120 days ago are still alive, and so forth. Of cells born 110 days ago (i.e., h/24 = 110), 84% are still alive at sampling. It is curious that half of the sampled 110 day-old cells would have lived longer than 120 d if not removed from circulation by the blood draw. This has no effect upon the HbA1c test. I used a spreadsheet to do the analysis. Obviously, I could not do an infinite number of calculations, like one for each millisecond. So I grouped the cells by day. Day #1 comprised cells from zero days old (i.e., h/24 = 0) to one day old (i.e., h/24 = 1). Day #120 comprised cells from 119 to 120 days old. I estimated the fractions of death and survival by using the midpoint of each group and a table of the normal distribution. Finally, the amount of HbA1c lost in dead cells had to be subtracted from the original model of table 1. This impacted all four months, since the dead cells were simply not circulating at sample time. That some cells survive > 120 d means that some cells from month 5 will survive until sampling. This was duly accounted for. Table 8 shows the results of analysis.

Figure 11. Hypothetical death and survival shown by two curves. Note that there are essentially no deaths until 90 days which is -3 standard deviations from the mean.
Table 8. HbA1c Under 120 d Mean and 10 d Standard Deviation, non-cumulative
| Birth month | A1c made 5th m ago | A1c made 4th m ago | A1c made 3rd m ago | A1c made 2nd m ago | A1c made 1st m ago | Total A1c |
| 5th m ago | 0.027 (a) | 0.132 | 0.132 | 0.132 | 0.132 | 0.555 |
| 4th m ago | 0.395 | 0.868 | 0.868 | 0.868 | 2.99 | |
| 3rd m ago | 0.50 | 1.00 | 1.00 | 2.50 | ||
| 2nd m ago | 0.50 | 1.00 | 1.50 | |||
| 1st m ago | 0.50 | 0.50 | ||||
| Total A1c | 0.027 | 0.527 | 1.50 | 2.50 | 3.50 | 8.05 |
The total HbA1c in table 8 is 8.05 relative units compared to 8.00 units in table 4. It seems that the loss of some month 4 cells is compensated by gaining some viable month 5 cells. A mathematician would have known this as soon as he or she looked at figure 11 and considered the symmetry of the bell-shaped curve. This compensation is complete in regard to HbA1c formed during the first through third months ago, where the cells born the fourth month ago lose 0.132 units which is exactly replaced by the cells born the fifth month ago. The addition of cells born the fifth month ago does slightly increase the HbA1c to 8.05 relative units, as the few surviving fifth month cells overcompensate in making HbA1c during the fourth and fifth months ago. The 0.027 figure in table 8 is very low because (1) only a few cells survived and because (2) they were mostly born close to the end of the month so had little exposure to plasma glucose in their birth month. With a mean life of 120 d, a uniform lifespan and a lifespan with standard deviation of 10 d give the same HbA1c result.
The Research Front
There are important research fronts in the study of glycohemoglobin. Besides clarification of RBC lifespan, there are questions about the genetic basis of glycohemoglobin variation. There are high glycators and low glycators who glycate more or less Hb than their plasma glucose predicts. This is quantified by the hemoglobin glycation index (HGI). There is a glycation gap characterized by a discordance between plasma protein glycation and Hb glycation. There are questions about differences in intracellular RBC glucose concentration in response to the same plasma glucose level. Some are saying that glycation in diabetics reduces RBC lifespan making the HbA1c results erroneously low; therefore, diabetic HbA1c results should be even higher.(7,8) This is big as it could lead to difficulty in diagnosis of diabetes when HbA1c is near the normal-diabetic threshold. There is Hb loss in older RBCs due to vesiculation. And, finally, there is a slim possibility that deglycation of HbA1c in older RBCs may affect results. The answers will affect modeling and improve clinical interpretation.
References
1. Nathan D M, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine R J. Translating the A1c assay into estimated average glucose values. Diabetes Care. 2008; 30(8): 1473-1478. doi: 10.2337/dc08-0545
2. Mahdi Kahrom. Mashhad University of Medical Sciences, Iran. An innovative mathematical model: a key to the riddle of HbA1c. International Journal of Endocrinology, vol. 2010. Article ID 481326, 6 pages, 2010. doi: 10.1155/2010/481326
This article models the change in mean plasma glucose and HbA1c following an
effective change in therapy. It relies upon two HbA1c assays, one before and one after
the new therapy and models the time after the new therapy and before the second
HbA1c assay.
I have not seen this idea elsewhere. Simple rearrangement of my equations used in getting
the weighted average will give the same information. His derivation is different. It is a
simple but elegant algebraic approach; however, there are about four typos in a page of
manipulations. The final equations are correct except, really, the equation on error.
3. Julia Korell, Carolyn V. Coulter, Stephen B. Duffull. Design of survival studies for red blood cells. Abstracts of the Annual Meeting of the Population Approach Group in Europe. 2010. Page 19 (2010)
Abstr 1701 [www.page-meeting.org/?abstract=1701]
4. Cohen R M, Franco R S, Khera. P K, Smith E P, Lindsell C J, Ciraolo P J, Palascak M B, and Joiner CH. Red cell life span heterogeneity in hematologically normal people is sufficient to alter HbA1c. Blood. 2008; 112: 4284-4291. doi: http://dx.doi.org/10.1182/blood-2008-04-154112
5. Robert M. Kalicki, Rocío Lledó-García, Mats O. Karlsson. Modeling of red blood cell (RBC) lifespan (LS) in a hematologically normal population. Abstracts of the Annual Meeting of the Population Approach Group in Europe. 2009. Page 18 (2009) Abstr 1677 [www.page-meeting.org/?abstract=1677]
6. Furne, J K, Springfield, J R, and Levitt, M D. Simplification of the end-alveolar carbon monoxide technique to assess erythrocyte survival. The Journal of Laboratory and Clinical Medicine. 2003, 142(1): 52-57. Abstract at: http://www.journals.elsevierhealth.com/periodicals/ymlc/article/S0022-2143(03)00086-6/abstract
7. Virtue, MA, Furne J K, Nuttall F Q, and Levitt M D. Relationship between GHb concentration and erythrocyte survival determined from breath carbon monoxide concentration. Diabetes Care. 2004; 27(4): 931-935
doi: http://dx.doi.org/10.2337/diacare.27.4.931
8. Cohen, R M, Franco R S, and Joiner C H. Is poor glycemic control associated with reduced
red blood cell lifespan?
Diabetes Care. 2004; 27(4): 1013-1014. doi: http://dx.doi.org/10.2337/diacare.27.4.1013
9. Goldstein, D E, Little, R R, Lorenz, R A, Malone, J I, Nathan, D, Peterson, C M, and
Sacks, D B. Tests of glycemia in diabetes. Diabetes Care. 2004; 27(7): 1761-1773.
doi: http://dx.doi.org/10.2337/diacare.27.7.1761
APPENDIX
A Graph Comparing 90 and 120 Day Lifespans per Relative Numbers of Tables 4 and 5.

The slope of the 3-month graph is greater by 1/3 than that of the 4-month graph. This was mentioned earlier. Why is this so? It is not due to any disparity in the rate of glycation of individual RBCs, for figure 10 shows that individual RBCs follow the same path no matter what the lifespan. One could argue that without the increase of slope the total area of the 3-month graph would be 4.5% instead of 6.0%, and that because 6.0% is the right amount (per figure 10), we must increase the slope to 4/3. This is true, but not satisfying. A deeper understanding involves the conversion of percent glycation of individual cells to percent glycation of total blood HbA. Consider a group of cells aged 0-1 month. Their within-the-cell glycation ranges from 0% to 4% with an average of 2%. If the lifespan is four months, we divide 2% by four to obtain the percentage glycation of total blood HbA. This 0.5% is represented by the area under the green line from 0 to 1 month. This is a triangular area of 1 x 1 / 2 = 0.5%. But if these cells have a three month lifespan, we divide 2% by three to obtain the percentage glycation of total blood HbA. This 2/3% is the area under the black line from 0 to 1 month, (1 x 4/3) / 2 = 2/3%. It seems like an artifact of the grouped-cell graph, but really it is not.
A Graph of High Sugar in the Last Month per Relative Numbers of Table 7.
Graph showing month in which HbA1c is formed. This graph is drawn with the x axis having the same meaning as in figure 5. The first month ago is to the right. It would look very different if the x axis were cell age.
By now, you know I’m crazy about graphs. I could launch a verbose discourse on the differences between individual cell and grouped cell graphs. I’ll spare you. I will dwell on the graph above in which increased sugar level causes an increased slope from three to four months. It also causes the vertical line which represents the cells alive at 3.00 months to more than double its height at exactly 3.00 months. Then, this line sweeps to the right forming the yellow rectangle. On top of this rectangle, the yellow triangle is formed by the combination of new cell birth and the new sugar level.
A Graph of High Sugar 4th Month Ago per Relative Numbers of Table 6.
Graph showing month in which HbA1c is formed. This graph is drawn with the x axis having the same meaning as in the last graph above. The first month ago is to the right. It would look different if the x axis were cell age.
The total area is much less than in the preceding graph, just as a comparison of tables 6 and 7 dictates.
Estimating the Effect of a Change in Therapy. This gives the same results obtained by
Dr. Mahdi Kahrom,(2) although the equations are different. Additionally, I have extended the concept to lifespans other than four months. When a patient has just had a HbA1c test and is prescribed new therapy, his physician may wish to estimate the effect of the therapeutic change without waiting four months to do the next HbA1c test. Presumably, this would be when the patient has very poor glycemic control and/or the new therapy is expected to be markedly efficacious. A reasonable presumption of two levels of stable plasma glucose is requisite: one level for the four months before the HbA1c test and the second level for the time since the HbA1c test, coinciding with the time since the start of the new therapy. Simply run a second HbA1c assay and apply the equation.
The central idea behind weighting is to calculate the amount of exposure of RBCs to a certain plasma glucose level. The unit is cell*exposure days or cell*exposure months or an analogous unit using some other time span. When an RBC is exposed to a stable glucose for 2 months, we have 2 cell*exposure months. Ten RBCs exposed for 1 month gives 10 cell*exposure months and so on. Having nicely defined this, we are putting it in mothballs, for we can use any unit proportional to cell*exposure days. Let us use area, since we have so many examples in the graphs already presented. We want the area, month by month, for four months when the sugar concentration is constant. Figure 5 gives what we want. The area above (formed) 4th month ago is 1/2, ((1x1)/2 = 1/2)), and above the third through 1st months ago it is 1 1/2, 2 1/2, and 3 1/2, respectively. Double these for 1,3,5,and 7 and we have the weighting factors used earlier.
Draw yourself a little right triangle with a base of 4 months and an altitude of whatever (for the altitude will not change the proportionality we are looking for).
We are at month 4, and have just done a second A1c. The first A1c was done 45 d ago at 2.5m. The large triangle shows the cells for the second A1c, not the first. Say the first A1c was a harmonized 10% and second a harmonized 8.5%.
Our first equation is:
(3.125 Hold + 4.875 Hunknown) / 8.0 = Hnew (1)
(3.125 x 10% + 4.875 Hunknown) / 8 .0 = 8.5% (2)
4.875 Hunknown = 8.0x 8.5% - 3.125 x 10% (3)
Hunknown = 7.54% (4)
Now, to check results by plugging back into eq 1:
(3.125 x 10% + 4.875 x 7.54%) / 8 = ?, = 8.51% = Hnew. Perfect.
A more general equation is:
((L - m)2 Hold + (2Lm - m2) Hunknown) / L2 = Hnew, (5)
where L is the lifespan and m is the number of months between the two A1c tests
and where m2, L2 and so forth means m squared and L squared, etc.
Rearrangement gives:
Hunknown = (L2 Hnew - (L - m)2 Hold) / (2Lm - m2 ) (6)
Now it might be felt that the patient’s RBC lifespan is somewhat less than 4 months. If so, use the general equation with L < 4. (Doing this does not "correct" the HbA1c numbers to the values they would have under a 120 d lifespan. Hold, Hnew, and Hunknown will all be lower than long-term average plasma glucose would predict.) Let Hold be 10% and Hnew 8.5%, again.
Let L = 3 and m = 1.5 :
Hunknown = (9 x 8.5 - 2.25 x 10) / 6.75 = 8.0 (7)
To leave a comment, open the comment box by clicking on the word "comments." Choose "anonymous" from the drop down list. Then, type your comment in the box and click "post." You may leave your name or any other identifying information as part of your comment. If your comment does not then appear, it is because I am moderating comments for offensive language. In that case, it should be posted in a day or two. It is a shame that such oversight is often required in this day. I should be able to give your comment a page of its own. You may have to "join" the blog in order for me to do this. (I am new to this site and don't know the details.) Thank you, Tom
WORK IN PROGRESS. COMPLETION CA 1-31-12




3 comments:
very nice work, but long, tom
I want traffic.--tlk
ok, i totally agree :)
Post a Comment